podiatry
Heel Pain
When walking, your heels repeatedly hit the ground with considerable force. They have to be able to absorb the impact and provide a firm support for the weight of the body.
When pain develops in the heel, it can be very disabling, making every step a problem, affecting your posture.
Common Symptoms
Heel Spurs - the pain is usually worst on standing, particularly first thing in the morning when you get up. It is relatively common, though usually occurring in the over forty's age group. There are no visible features on the heel but a deep localised painful spot can be found in or around the middle of the sole of the heel. Although it is often associated with a spur of bone sticking out of the heel bone (heel spur syndrome), approximately ten per cent of the population have heel spurs without any pain.
Heel Bursitis - pain can be felt at the back of the heel when the ankle joint is moved and there may be a swelling on both sides of the Achilles tendon. Or you may feel pain deep inside the heel when it makes contact with the ground.
Heel Bumps - recognised as firm bumps on the back of the heel, they are often rubbed by shoes causing pain.
Plantar fasciitis
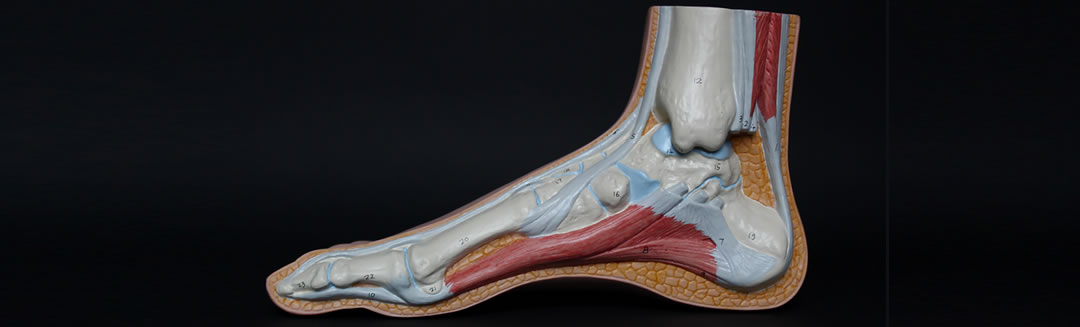
Plantar fasciitis is inflammation of the thick tissue on the bottom of the foot. This tissue is called the plantar fascia. It connects the heel bone to the toes and creates the arch of the foot.
Causes, incidence, and risk factors ... Plantar fasciitis occurs when the thick band of tissue on the bottom of the foot is overstretched or overused. This can be painful and make walking more difficult.
Risk factors for plantar fasciitis include:
- Foot arch problems (both flat feet and high arches)
- Obesity or sudden weight gain
- Long-distance running, especially running downhill or on uneven surfaces
- Sudden weight gain
- Tight Achilles tendon (the tendon connecting the calf muscles to the heel)
- Shoes with poor arch support or soft soles
Plantar fasciitis most often affects active men ages 40 - 70. It is one of the most common orthopaedic complaints relating to the foot.
Plantar fasciitis is commonly thought of as being caused by a heel spur, but research has found that this is not the case. On x-ray, heel spurs are seen in people with and without plantar fasciitis.
Symptoms
The most common complaint is pain and stiffness in the bottom of the heel. The heel pain may be dull or sharp. The bottom of the foot may also ache or burn.
The pain is usually worse:
- In the morning when you take your first steps
- After standing or sitting for a while
- When climbing stairs
- After intense activity
The pain may develop slowly over time, or suddenly after intense activity
Ingrowing Toenails
What is it?
An ingrowing toenail is one that pierces the flesh of the toe. It can feel as if you have a splinter, and can be extremely painful. In more severe cases, it can cause pus and bleeding. Ingrowing toenails most commonly affect the big toenail, but can affect the other toes too.
A nail that is curling (involuted or convoluted) into the flesh but isn’t actually piercing the skin isn't an ingrowing toenail, but can feel very painful and also appear red and inflamed as well.
Who gets it?
Active, sporty people are particularly prone, because they sweat more. Younger people are more likely to get it (as they pick their nails more, compared to older people who may not reach their toes!) Women often develop them as a result of cutting nails too low in order to relieve the pressure and discomfort of an involuted nail.
Is it serious?
If left untreated, the infection can spread to the rest of the toe. The quicker you treat it, the less painful the treatment.
What causes it?
There are many genetic factors that can make you prone to ingrowing toenails such as your posture (the way you stand), your gait (the way you walk), a foot deformity such as a bunion, hammer toes or excessive pronation of the feet (when your foot rolls in excessively). Your nails may also naturally splay or curl out instead of growing straight, encouraging your nail to grow outwards or inwards into the flesh. Other irritating factors may be medication, direct or historical trauma to the nail bed/matrix, fungal and other infections. Tight footwear, tight hosiery and tight socks can also push your toe flesh onto the nail so that it pierces the skin.
Diabetic Foot Assessment & Care
Many people with diabetes (both type 1 and type 2) know that they should take care of their feet but do not always know why. Understanding how and why foot problems can develop helps to prevent them.
High blood glucose levels can cause damage to the nerves in your body which can stop messages getting to and from your brain. The nerves that are most likely to be affected are the longest ones including those to your feet and legs. This is also known as neuropathy.
Managing your diabetes with a healthy lifestyle and maintaining good control of your blood glucose levels will help to prevent problems with the blood vessels that supply your legs and feet. Good regular footcare will prevent the build-up of hard skin and checking your feet daily for any skin damage or injury is advisable.
If you do have a problem, need advice on foot-wear or simply feel a regular check up from a professional to help with your foot check would put your mind at rest, contact a health care professional who has been specially trained such as a podiatrist.
Verrucae
Verrucae are warts that can be found anywhere on the foot but commonly occur on the soles of the feet. They can even be found around the edges of nails. They are caused by the Human Papilloma Virus (HPV) and are passed from person to person by direct contact. The virus is thought to thrive in moist, damp environments such as swimming pools, changing room floors and communal shower areas. If an infected foot deposits skin cells onto the floor then it is possible to walk across the same floor and pick up the virus, especially if your skin is scratched or cut.
Verrucae are harmless but hard skin can build up over them causing some discomfort and they can spread quickly. Minimise your chances of catching verrucae by keeping your feet in a healthy condition. Use creams and lotions if your skin is dry and use surgical spirit if your feet are excessively sweaty. Treat other conditions such as Athlete's foot, which can damage the skin surface. Wear flip-flops in communal changing areas and don't share towels. Verruca socks can help avoid passing on the virus and also can be worn as a preventative measure.
To seek treatment contact a Podiatrist who will carry out a general and foot health assessment in order to decide on a treatment plan.
Athletes Foot
Athlete’s foot is a fungal infection. It can lead to intense itching, cracked, blistered or peeling areas of skin, redness and scaling. It can occur on moist, waterlogged skin especially between the fourth and fifth toes, or on dry, flaky skin around the heels or elsewhere on the foot.
It’s caused by a number of fungal species which you can pick up from places such as pools, showers and changing rooms, or anywhere where you may walk around barefoot. The fungus on each bit of skin that falls away from someone else’s feet can be picked up by you if you’re prone.
Once your feet have been contaminated, the warm, dark and sweaty environment of feet cramped in shoes or trainers provides the ideal breeding ground for the fungus. However, athlete’s foot also occurs in dry, flaky areas. It’s quite common in summer sandal-wearers. The sun makes your skin dry out, so it loses its natural protective oils; this combined with the constant trauma from sandals makes them more prone to infection.
If left untreated, the fungus can spread to the toe nails, causing thickening and yellowing of the nail, which is much harder to treat. Fungal infections are highly contagious and can spread to anywhere on your skin – to your scalp, hands and even your groin, especially if you use the same towel for your feet as for the rest of your body.
There are many things you can do to make your feet less hospitable to fungal infections: Firstly, change your footwear on a regular basis.. It takes 24-48 hours for shoes to dry out properly, so alternate your shoes daily. You should also change your socks every day too.
You may be able to get rid of athlete’s foot on your own but a podiatrist can help you pinpoint the best treatment for your particular type of athlete’s foot. They can also help if the fungal infection has spread to your nails by reducing the thickness and cutting back the nails, thereby exposing the infected nailbed to a lighter, cooler environment.
Nail infections don’t respond to topical treatments. You need oral medication (i.e. tablets) to kill the fungus in nails. If the fungus is only in the nail and not elsewhere, it is probably caused by an injury. An injury allows the fungus to creep in and multiply under the nail. This can affect the substance of the nail which may become crusty, discoloured and deformed. This oral medication needed, however, can have side effects, particularly if you have other medical conditions or are on other medication. Your GP or podiatrist may recommend that you don’t take it.
Gait / Walking Analysis / Orthotics
Gait analysis is the foundation of knowledge specific to podiatrists. Biomechanics is a subsection of gait/walking. Biomechanics is concerned with preservation, restoration and development of the function of the foot and its associated structure. Biomechanics refers to an understanding of the mechanics in the body and podiatrists use this to diagnose and treat the lower limb. This is a subject that interests a lot of practitioners and covers a number of areas of practice.
One area of clinical practice that focuses on biomechanics is sports injuries. There is currently a big demand for podiatrists to treat sports injuries. Most of those working in this area are self-employed private practitioners. The work can involve working with individual athletes or working for sports teams e.g. rugby or football clubs.
There are many biomechanical investigations podiatrists use to help them assess and evaluate the patients they treat. A lot of biomechanical problems are treated with orthotics. These are custom made insoles specifically for each patient that aim to improve function and reduce symptoms. Podiatrists use orthotic labs where orthotic technicians produce the device based on the prescription written by the podiatrist.
Children's Feet
Podopaediatrics is the assessment and treatment of children's feet. There is rapid musculoskeletal growth in children and is a key opportunity for podiatrists to assist in development. In some cases heel cups, heel raises and in-shoe orthotics/insoles are indicated at an early stage.
When treating children, it is important to remember that they are not small adults, however, in some cases can develop early onset adult type changes within the foot. They are physically and emotionally different and, most importantly from the registered podiatrist’s point of view, they grow. Many of the problems found on the paediatric foot care associated with growth, overuse, weight gain and postural change. The podiatrist can help your child by providing an initial diagnosis and then either managing the condition or referring to an appropriate consultant. Treatment may take the form of footwear prescription or advice, biomechanical assessment – which determines the normal and abnormal functioning of the foot and lower limbs and often involves the provision of orthoses (special insoles).
Footwear Advice
We provide advice on all ranges of shoes from street wear, corporate and sports/running shoes.
Achilles Rupture
The Achilles tendon is an important part of the leg. It is located just behind and above the heel. It joins the heel bone to the calf muscles. Its function is to help in bending the foot downwards at the ankle (this movement is called plantar flexion by doctors).
If the Achilles tendon is torn, this is called an Achilles tendon rupture. The tear may be either partial or complete. In a partial tear, the tendon is partly torn but still joined to the calf muscle. With complete tears, the tendon is completely torn so that the connection between the calf muscles and the ankle bone is lost .As with any muscle or tendon in the body, the Achilles tendon can be torn if there is a high force or stress on it.
The Achilles tendon can also be damaged by injuries such as falls, if the foot is suddenly forced into an upward pointing position - this movement stretches the tendon. Another possible injury is a deep cut at the back of the ankleThis condition should be diagnosed and treated as soon as possible, because prompt treatment probably improves recovery., which might go into the tendon. There are two options for treatment. One option is an operation to surgically repair the tendon. The surgeon sews together the torn ends of the Achilles tendon, and perhaps may also use another tendon or a tendon graft to help with the repair. A plaster cast or brace is needed after the operation.
The other option is to allow time for the tendon to heal naturally, resting it in a brace or plaster cast. This is called conservative treatment. If the tendon does not heal on its own, a surgical repair can then be done later.
Both options will involve having a plaster cast or brace (orthosis) for about eight weeks, to protect the tendon while it heals. The plaster or brace is positioned so that.he foot is pointing slightly downwards, which takes the strain off the tendon.
Traditionally, crutches were used to keep weight off the leg during the first few weeks of treatment. Now there is a trend towards early mobilisation. This involves fitting a plaster or brace which you can walk on. It is more convenient because you do not need to use crutches. Physiotherapy is often provided as well.

Achilles tendonitis
This is inflammation of the tendon, usually resulting from overuse associated with a change in playing surface, footwear or intensity of an activity.
The Achilles tendon is surrounded by a connective tissue sheath (paratenon, or 'paratendon'), rather than a true synovial sheath. The paratenon stretches with movement, allowing maximum gliding action. Near the insertion of the tendon are 2 bursae, the subcutaneous calcaneal and the retrocalcaneal bursae.1
Gradual onset of pain and stiffness over the tendon, which may improve with heat or walking and worsen with strenuous activity.Tenderness of the tendon on palpation. There may also be crepitus and swelling.
The patient should abstain from aggravating activities, but with a minimum of rest in order to preserve overall fitness. Possible treatments are: non-steroidal anti-inflammatory drugs (NSAIDs), ice, rest, increased warm-up/stretching exercises, physiotherapy and heel lifts (orthotic devices - used on both sides to prevent a gait imbalance.).
Bunions
Recent research from the Society of Chiropodists and Podiatrists revealed that 80 per cent of women suffer from foot problems and 15 per cent from bunions. Contrary to popular opinion, bunions are not actually caused by shoes. They are most often caused by a defective mechanical structure of the foot, which is genetic, and these certain foot types make a person prone to developing a bunion.
Shoes themselves are not the sole cause of bunions, but wearing shoes that squeeze the forefoot, crowding the toes together can exacerbate the underlying condition, causing pain and deformity of the joint (known as Hallux Valgus). Some treatments can ease the pain of bunions by relieving the pressure on the foot and reduce possible pressure sores and ulcers. Podiatrists can also prescribe orthoses to prevent the condition from becoming worse but only surgery can correct the defect.
Structural Disorders
Flat Feet
Flat feet is a condition in which the foot doesn't have a normal arch. It may affect one foot or both feet. Most people have a gap between the inner side of the foot and the ground when they are standing. This is referred to as an "arch". Feet that have a low arch or no arch at all are referred to as flat feet or fallen arches. Symptoms may include pain or tenderness along the arch and problems such as calf pain, knee pain and hip pain may be present.
High Arched Feet
This condition is the opposite of flat feet and is often associated with a problem of nerves to the foot, although this is not always the case.
Hammer Toes
Hammertoe is a contracture (bending) of one or both joints of the second, third, fourth, or fifth (little) toes. This abnormal bending can put pressure on the toe when wearing shoes, causing problems to develop. Hammertoes often start out as mild deformities and get progressively worse over time. In the earlier stages, hammertoes are flexible and the symptoms can often be managed with non-invasive measures.
The most common cause of hammertoe is a muscle/tendon imbalance. This imbalance, which leads to a bending of the toe, results from mechanical (structural) changes in the foot that occur over time. Hammertoes may be aggravated by shoes that don’t fit properly. Occasionally, hammertoe is the result of an earlier trauma to the toe. In some people, hammertoes are inherited.
Non invasive measures (non surgical) that can be taken include changes in footwear, orthotic devices, injection therapy, anti-inflammatory medication such as ibuprofen and splinting/strapping.